Presidents' Lecture
Evidence-Based Medicine & The GRADE Framework
The Past, Present, and Future
Gordon Guyatt
Professor of Medicine and Health Research Methods
McMaster University
Sponsored by PSW Science Members Larry Millstein & Robin Taylor
About the Lecture
Evidence-based medicine (EBM) has achieved wide acceptance, including its incorporation as a required component of undergraduate and postgraduate health sciences training programs throughout North America and, to a lesser extent, internationally. It is now broadly recognized as a core element of medical practice. As a result, only clinicians nearing retirement can readily recall a time before evidence-based medicine was part of routine training and care.
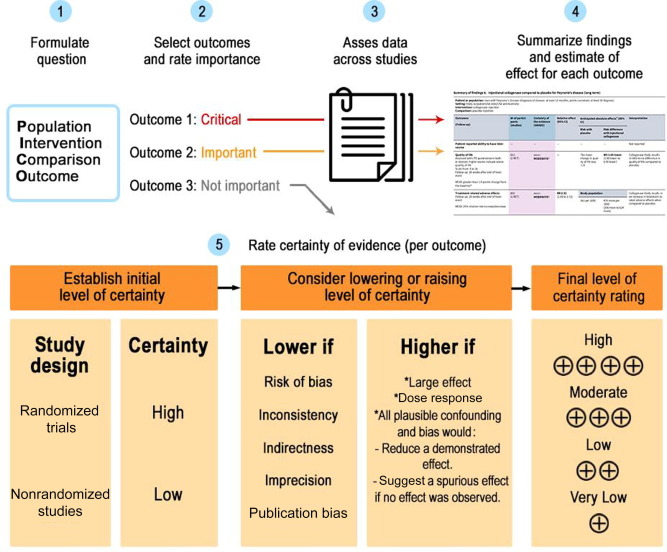
The GRADE approach—*Grading of Recommendations, Assessment, Development, and Evaluation*, a framework for rating certainty of evidence and moving from evidence to recommendations—has reshaped how systematic reviews are conducted and interpreted. It has become a standard component of clinical practice guidelines and health technology assessments, which evaluate the clinical and economic value of health interventions. *UpToDate*, an online clinical decision-support resource, has become a widely used evidence-based reference for clinicians. During the COVID-19 pandemic, evidence-based medicine performed well in guiding individual patient care. The MAGIC initiative (*Making GRADE the Irresistible Choice*) has provided leadership in strengthening how evidence is produced, summarized, and applied across the healthcare ecosystem.
Despite these advances, evidence-based medicine faces persistent challenges. In the public health response to COVID-19, decision-makers often failed to clearly communicate evidence-based principles and, at times, disregarded them. Many EBM educators have been slow to accept that most clinicians will not critically appraise original research articles themselves; and that, instead, education should focus on helping clinicians correctly interpret research results and understand their implications. Shared decision-making—an approach in which clinicians and patients work together to make healthcare choices based on evidence and patient values—remains uncommon in routine practice, despite existing concepts for implementing it efficiently.
In the processing and presentation of evidence, the field has struggled to balance simplicity with necessary complexity. Methodological sophistication has increasingly come at the expense of usability for everyday clinical and public health practice. The global EBM community needs to shift attention away from increasingly technical methods and toward practical solutions that better serve clinicians and policymakers. The GRADE framework has become difficult to use in practice, the Cochrane *Risk of Bias 2* tool for randomized trials is hard to interpret, and *ROBINS-I* (a tool for assessing bias in non-randomized studies) has proven particularly challenging. Newer approaches, such as *ROBUST-RCT* for assessing risk of bias in randomized trials and *Core GRADE*, aim to simplify and improve how evidence quality is assessed and applied.
This lecture will discuss the advances EBM has brought about in clinical outcomes, some, the challenges to fuller implementation and further improvements, and approaches to meeting those challenges and to improving outcomes for patients universally.
References
Wikipedia / Gordan Guyatt: https://en.wikipedia.org/wiki/Gordon_Guyatt
Oral History discussion: https://edhub.ama-assn.org/jn-learning/video-player/6391356
About the Speaker

Gordon Guyatt is Professor of Medicine and of Health Research Methods at McMaster University, where he has spent his academic career as a clinician, investigator, and educator. He previously served in senior academic roles within the Department of Medicine and the clinical epidemiology program.
Gordon’s research focuses on clinical epidemiology, evidence-based medicine (EBM), research methodology, and outcomes research. It integrates methodological development with practical clinical questions. He has worked to improve how clinical evidence is generated, appraised, and applied to clinical care and health policy. A consistent emphasis of his work is the measurement and use of patient-important outcomes rather than surrogate endpoints.
Gordon is well known for coining the term “evidence-based medicine” (EMB) and for founding and building an approach to medical education and practice that integrates research evidence with clinical expertise and patient values. He played a leading role in developing the “Grading of Recommendations, Assessment, Development and Evaluation” (GRADE), a systematic framework used in clinical medicine and public health to rate the certainty (quality) of evidence and the strength of healthcare recommendations. And he was instrumental in the creation of the “Users’ Guides to the Medical Literature”, now widely used in teaching how to evaluate and best use medical research in clinical decision-making.
Gordon in an author on more than 2,000 peer-reviewed publications and an author or editor of several books. His work has been cited extensively in the scientific literature. According to the Web of Science/Google scholar his publications have been cited over 235,000/350,000 times, with H-Indices of 225/313. Indeed, Gordon is one of world’s 20 most cited living scientists in any area, among the top 10 in health sciences and, as well, is Canada’s most cited scientist.
Gordon has received many national and international honors for his contributions to medicine and public health, including to name just a few: the Wallace H. Coulter Distinguished Lecture Award, the Queen Elizabeth II Diamond Jubilee Medal, induction into the Canadian Medical Hall of Fame, designation as Canadian Institutes of Health Research Researcher of the Year, the Canadian Society of Internal Medicine Senior Investigator Award, the Einstein Foundation Award for Promoting Quality Research, and the international Henry Friesen Award. Gordon is a Fellow of the Royal Society of Canada and an Officer of the Order of Canada.
Gordon earned a BA in Psychology, an MD, and an MSc in Clinical Epidemiology at McMaster University.
X: https://x.com/GuyattGH
LinkedIn: https://t.co/U6a8xibEvR
Bluesky: https://bsky.app/profile/guyattgh.bsky.social
Minutes
On January 23, 2026, Members of the Society and guests joined the speaker for a reception and dinner at 5:45 PM in the Members’ Dining Room at the Cosmos Club. Thereafter they joined other attendees in the Powell Auditorium for the lecture proceedings. In the Powell Auditorium of the Cosmos Club in Washington, D.C., President Larry Millstein called the lecture portion of the 2,529th meeting of the Society to order at 8:06 p.m. ET. He began by welcoming attendees, thanking sponsors for their support, announcing new members, and inviting guests to join the society. Scott Mathews then read the minutes of the previous meeting which included the lecture by Bernard Carlson, titled “Tesla, Marconi, and the Invention of Radio”. The minutes were approved as read.
President Millstein then introduced the speaker for the evening, Gordon Guyatt, of McMaster University. His lecture was titled “Evidence-Based Medicine & The GRADE Framework”.
The speaker began by discussing EBM, or evidence-based medicine, saying that while it has changed the world, there is more work to be done. He described medical treatment before EBM as largely based on physiological rationale, clinical experience, and expert recommendations. He claimed that the first paper published on evidence-based medicine appeared in 1991, in the American College of Physicians Journal Club. He presented the original “Hierarchy of Evidence for Therapy”. In order of importance were: randomized trials, observational studies, basic research, and clinical experience. He discussed the Cochrane Collaboration, a British organization that performs systematic reviews and meta-analysis of published medical studies.
Guyatt presented an example of the importance of such systematic analysis by discussing a 1990 study on Thrombolytic Therapy. This study enrolled 40,000 patients, only 20,000 of which received the therapy, at least 10 years after the evidence demonstrated efficacy; meaning that 20,000 patients were denied an effective treatment because the statistics had not been evaluated. The speaker discussed the use of lidocaine in treating myocardial infarction; a common practice in the 1960’s and 70’s. He claimed that a meta-analysis performed in 1989 clearly showed no benefit, and likely showed harm.
The speaker then made the statement “Evidence does not make decisions, people do.” To demonstrate this principle, he conducted a poll of the audience, describing the risks and benefits associated with a particular treatment and asking how many adverse events they would tolerate per 100 patients. A small number of people indicated they would tolerate a small number of adverse events, while the majority of the audience said they would tolerate more than 20, clearly demonstrating a wide range of opinions with respect to the risk-benefit analysis. Guyatt showed actual data from both physicians and patients, again indicating a wide range of acceptable adverse events. Above 20 adverse events per 100 treatments, patients were 5 times more likely to accept the risk than physicians. The speaker said that physicians should not substitute their values and preferences for those of the patient.
Guyatt summarized the three principles of evidence-based medicine as follows:
• Some evidence is more trustworthy than other evidence
• Good clinical care requires systematic summaries of the best available evidence
• Evidence, by itself, is never sufficient
The speaker provided a history of the publications on EBM in medical journals: the first paper in 1991, a second paper in 1992, a Users’ Guide in 1993, and a 25-part series published in JAMA (Journal of the American Medical Association) completed in 2000. The 3rd edition of the Users’ Guides, in both long form and short summary, were published in 2015. Guyatt said that EBM has become a “core competency” in medicine, nursing, and rehab science. He said that by 2007, medical schools had to teach EBM in order to be accredited, and that it was widely considered to be one of the top 10 most important advances in medicine since 1840.
Guyatt then discussed some of the shortcomings or misgivings of EBM. He said that in the 1990’s he assumed that all medical students, upon completion of their residency, would be able to assess and critically appraise the methods and results of journal publications. He said that this was very unrealistic and found that very few could. By the early 2000’s, he and others in the EBM community concluded that not all practitioners need to appraise evidence “from scratch”.
The speaker described the GRADE system (Grading of Recommendations, Assessment, Development and Evaluation); a transparent, structured framework used in healthcare to rate the quality of scientific evidence and determine the strength of clinical recommendations. Guyatt described what was required to make the GRADE system “irresistible” to clinicians, patients, and developers. This included introducing “Rapid Recommendations”, creating an electronic platform, creating “decision aids”, and implementing platform trials with rapid meta-analysis. He described how GRADE and EBM performed during the COVID pandemic, saying that it produced unprecedented rapid production of evidence and rapid meta-analysis, leading to six classes of drugs and several vaccines within two years of the outbreak.
The speaker ended his talk by saying that there is now widespread recognition of the need for hard evidence, the standardization of evaluation metrics, and the systematic review and meta-analysis of that evidence, but that more work needs to be done in educating clinicians to evaluate research, and in the application of shared decision making.
The lecture was followed by a Question and Answer session.
A member asked if Guyatt has seen a generational shift, with younger practitioners being more able and willing to accept the suggested changes in methodology. Guyatt responded, “The answer is yes, and it has been fairly dramatic.” He said that in the beginning there was intense resistance, and that the widespread acceptance was at least partially due to older physicians retiring, and being replaced by the next generation.
A member asked “Is it wise to disregard physiological rationale?” Guyatt responded that EBM and GRADE do not suggest ignoring physiology, but they require randomized trials to verify the efficacy of any treatment, regardless of the rationale that motivated the treatment.
A member asked about both the risk of data overload and “bad actors” or misinformation. Guyatt responded that rapid meta-analysis has become so efficient that it is unlikely that we will “drown in data”. He said that he had the sense that the EBM community did not have good strategies for dealing with misinformation, but that he had no real evidence to support that conclusion.
A member on the live stream asked if people in the EBM field were aware of Dr. Ignaz Semmelweis, who proposed many of the ideas of evidence-based medicine 160 years ago, and then was committed to a mental institution. Guyatt said that it was a very famous story. He described how the “vitriol” Semmelweis experienced reminded him of the reaction of so many doctors in the early days of EBM. He said “Fortunately, insanity did not set-in, in my case.”
After the question and answer period, President Millstein thanked the speaker and presented him with a PSW rosette, a signed copy of the announcement of his talk, and a signed copy of Volume 17 of the PSW Bulletin. He then announced speakers of up-coming lectures and made a number of housekeeping announcements. He adjourned the 2,529th meeting of the society at 10:06 pm ET.
Temperature in Washington, DC: -2.8° Celsius
Weather: Mostly Cloudy/Windy
Dinner Attendance: 49
Lecture Attendance:
In person: 58
Live stream: 16
For a total of 74 viewers
Views of the video in the first two weeks: 144
Respectfully submitted,
Scott Mathews, Recording Secretary